Hypoxic Pulmonary Vasoconstriction
Hypoxic Pulmonary Vasoconstriction (HPV) is an physiological process that helps to balance ventilation and perfusion (V/Q) during states of decreased ventilation. This can occur during atelectasis, pneumonia, or COPD but we see it most pronounced during one-lung ventilation. The basic concept is the pulmonary vasculature clamps down on the arteries doing to parts of a lung (or a whole lung) that is hypoxic, reducing the amount of blood flow to that area. This allows for more of the pulmonary circulation to be directed towards healthy lung that has adequate levels of oxygen to be picked up by passing red blood cells. The other innate physiologic response the body has to hypoxia is in the carotid body, where there is an increase in ventilation in response to systemic arterial hypoxia.
We don’t always see HPV in pathological states. For example, we see it in utero with with fetal lungs being unventilated and having high pulmonary vascular resistance due to this. You also see it when climbing in altitude - a phenomenon known as High Altitude Pulmonary Edema (HAPE). The high resistance causes capillary leaking of fluid into the lungs that corrects with oxygenation, hyperbaric treatment, or rapid descent in altitude.
During single lung ventilation, a large portion of the operative lung will become hypoxic. This results in the doubling of pulmonary artery pressure (PAP) and tripling of PVR leading to a reduction of blood flow to the hypoxic lung from ~50% to ~30%. This response to hypoxia is specific to the pulmonary system. In fact, the opposite occurs in systemic circulation with vasodilation occurring in times/locations of hypoxia.
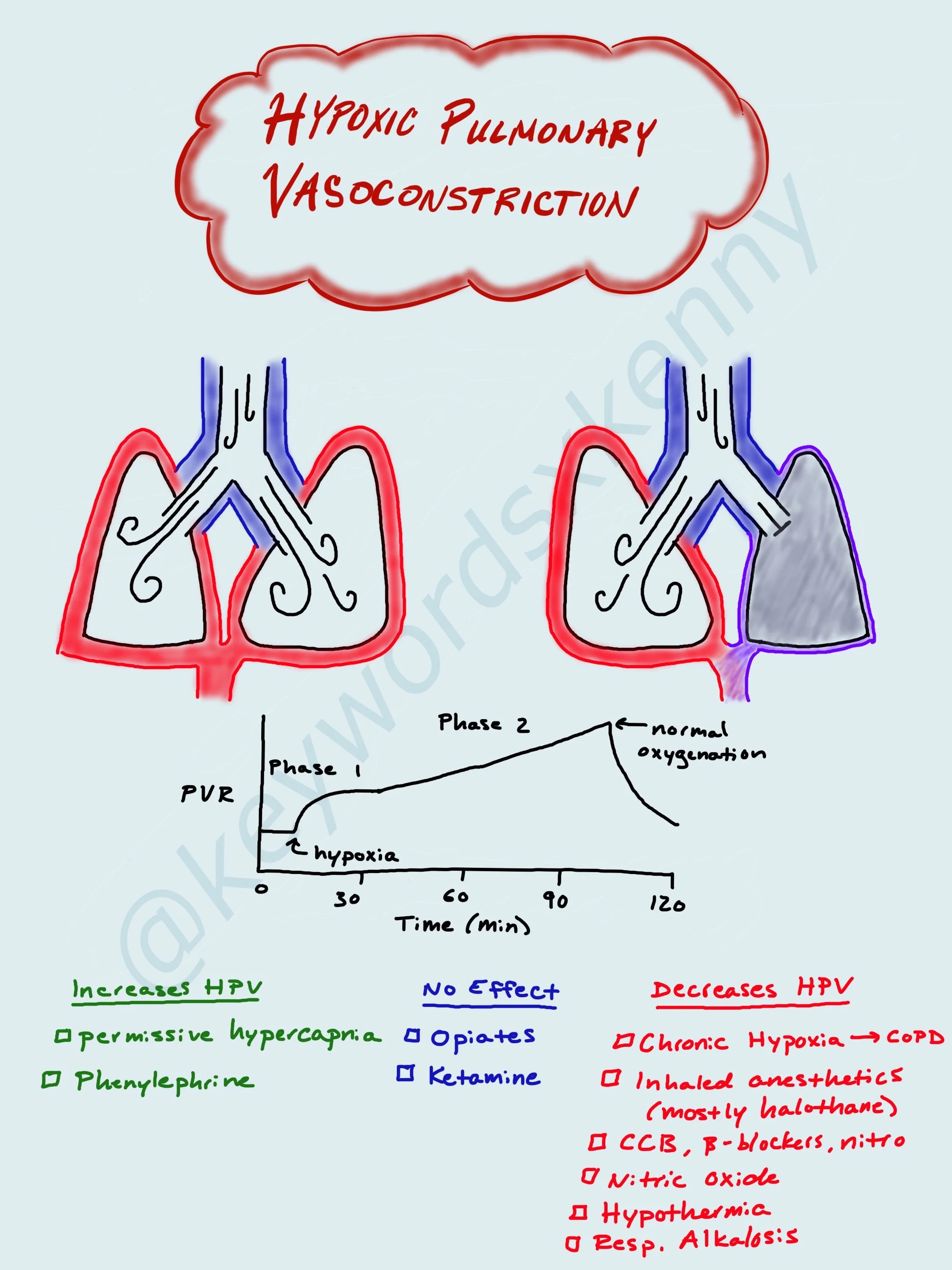
The HPV response comes from a low FiO2 in the pulmonary arteries. It starts to occur around 12% (room air O2 is 21%). The response is biphasic, with the first sharp increase in PVR occurring over the first 30 minutes of hypoxia. After a couple hours of hypoxia, the HPV can persist for hours even after normal oxygenation has been restored. Patients coming back for multiple surgeries involving single lung ventilation has an increased HPV response, with some hypothesizing that some of the original vasoconstriction never corrected and continued to shunt blood away from the diseased or nonventilated lung.
There are certain patients who have an exaggerated HPV response, as evident by some hikers having a more profound HAPE reaction. The cause is thought to be genetic, but not totally understood. There are other patients who have a diminished HPV response. This includes patients with cirrhosis or COPD who either have increased vasodilating mediators circulating in their blood or are chronically exposed to hypoxia, respectively. There are also medications that can decrease the HPV response. These include inhaled anesthetics (most seen with Halothane), calcium channel blockers, nitrates, and beta-blockers. Respiratory alkalosis can also blunt the HPV response.
During single lung ventilation, we rely on HPV to maintain normal systemic oxygenation. When patients have diseased states that hinder their response to hypoxia, our job is to maintain as much HPV as possible. This would include discontinuing any vasodilating medications mentioned above. In situations of hypoxia during single-lung ventilation, you can optimize the patient’s HPV with permissive hypercapnia, inhaled nitric oxide (vasodilated pulmonary vasculature to ventilated lung only), and possibly switching your inhaled anesthetics for IV anesthetics (although studies don’t show much of a difference here).