
Featured Posts
Looking for something specific?

Digoxin
Digoxin is a medication that is commonly used for congestive heart failure (CHF) and arrhythmias like atrial fibrillation or flutter with rapid ventricular rates (RVR). It has largely been replaced by medications that have a safe side-effect panel like beta-blockers and calcium channel blocks, but you will still see patients on this medication every now and then. Even though prescribing this medication is reserved for cardiology, it is still important for perioperative providers to understand how this medication works and why it is used.
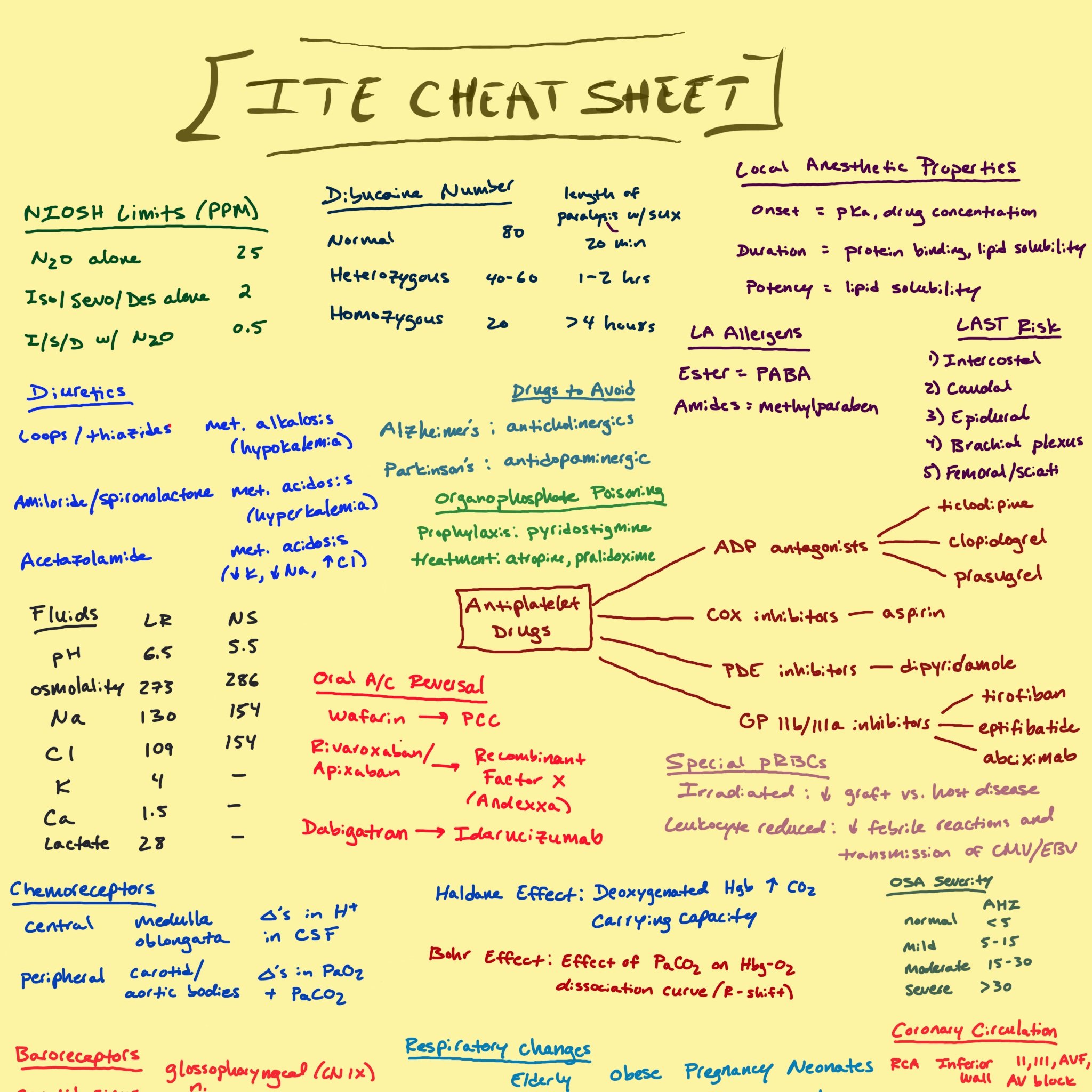
ITE Cram Sheets
The ITE (or In-Training Exam) is an annual exam for Anesthesiology trainees that tests their clinical knowledge. Residency programs typically use it as a benchmark for likelihood of passing the BASIC and ADVANCED Board Exams. These two sheets are designed to be high-yield cram sheets of factoids that I felt like were commonly tested and easy to memorize for the test.

Glucagon
Glucagon is a hormone in the body that helps maintain homeostasis, specifically regarding glucose (sugar) levels. While we sleep at night, our bodies are fasting and not taking in glucose or nutrition. Glucagon is able to maintain normal levels of blood glucose levels so that we don’t go into a state of hypoglycemia (low blood sugar).

Lumbar Spinal Drain
One of the more significant complications of thoracoabdominal aortic surgery is ischemic spinal cord injury (SCI). The result of this can be paralysis and lack of sensation to both lower extremities. This can present immediately after surgery (acute) or be delayed for several days (postponed). Placing a lumbar cerebrospinal fluid (CSF) drain can reduce the risk of SCI by reducing the intraspinal pressure (or ICP) and allowing more perfusion to the spinal cord. Spinal cord perfusion is determined by mean arterial pressure minus intracranial pressure (SCP = MAP - ICP). ICP can be replaced with central venous pressure (CVP) in this equation, depending on which is higher.

Hypoxic Pulmonary Vasoconstriction
Hypoxic Pulmonary Vasoconstriction (HPV) is an physiological process that helps to balance ventilation and perfusion (V/Q) during states of decreased ventilation. This can occur during atelectasis, pneumonia, or COPD but we see it most pronounced during one-lung ventilation. The basic concept is the pulmonary vasculature clamps down on the arteries doing to parts of a lung (or a whole lung) that is hypoxic, reducing the amount of blood flow to that area. This allows for more of the pulmonary circulation to be directed towards healthy lung that has adequate levels of oxygen to be picked up by passing red blood cells. The other innate physiologic response the body has to hypoxia is in the carotid body, where there is an increase in ventilation in response to systemic arterial hypoxia.

Extubation Criteria
A lot of attention is placed on intubations, however extubation of a patient is just as important and requires diligence and preparation in order to avoid complications. Routine extubation at the end of a surgical procedure is generally very safe, but it is reasonable to have back up equipment readily available or know where it is to grab in the case of needing to reintubate. If you go about this process in an organized and systematic manner, you can create a safe scenario for the patient to be transferred to the PACU for remainder of their recovery. Most providers pick up on this process quickly in training and do many of the right moves without thinking about it, but let’s review the steps that go into extubating a patient.
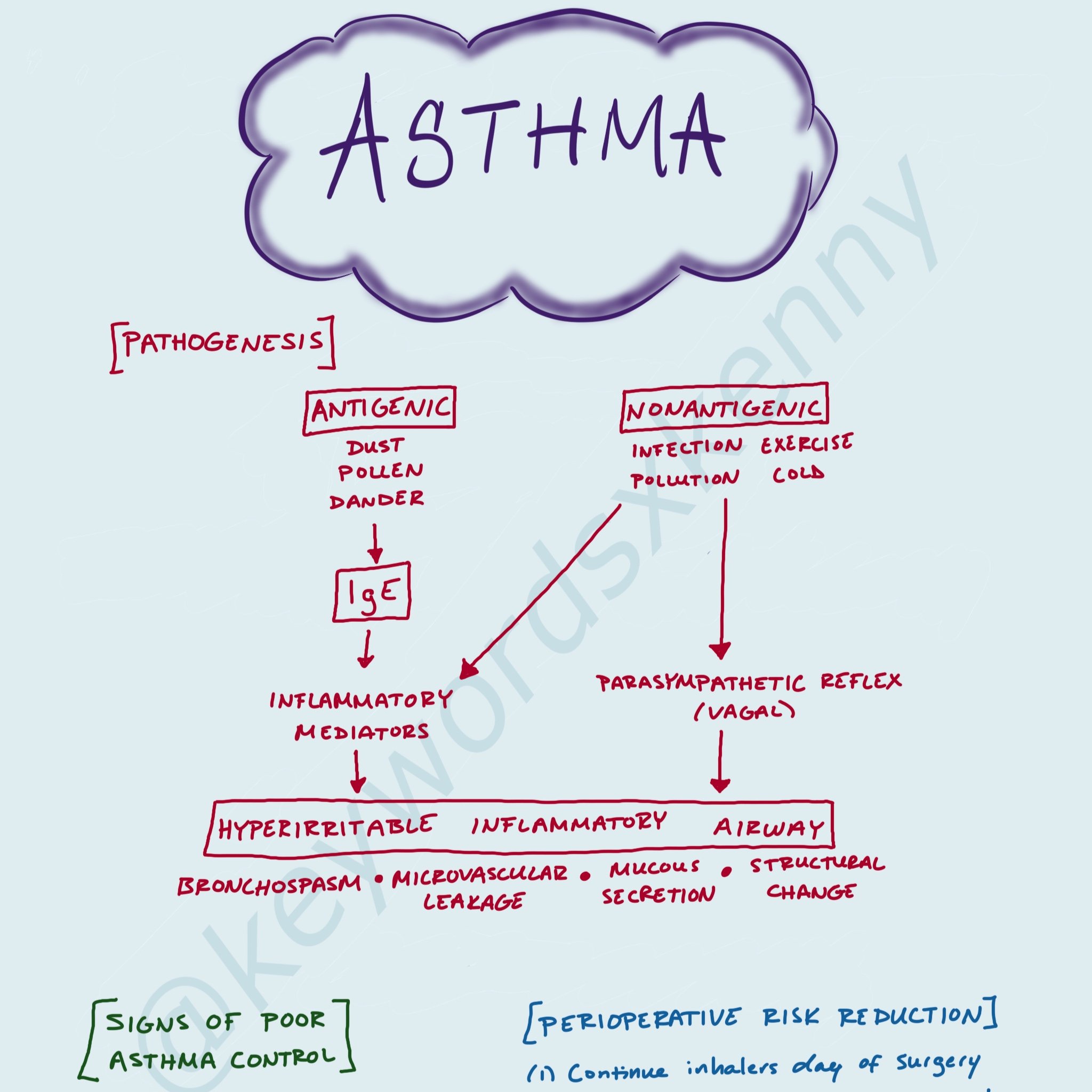
Asthma
Asthma is one of the most common chronic disease across the world. It affects around 300 million people. In the United States, it has a prevalence of 8.7% in adults and 8.2% in children. It can occur at all ages, but has a peak incidence between ages 5 and 9. Asthma is characterized as periodic episodes or attacks that result in difficulty breathing, coughing, and wheezing.

Treatment of Hyperkalemia
Recognition and treatment of hyperkalemia is crucial to avoid serious complications, such as death. The urgency needed to address this problem is based on a few factors: how fast the hyperkalemia developed, the current serum potassium level, the degree of signs/symptoms, and the underlying cause. Severe hyperkalemia is define as a serum potassium level of greater than or equal to 5.5 mEq/L. Concerning signs and symptoms include ECG changes (ie. peaked T waves, widened QRS, prolonged PR interval), neuromuscular weakness, and/or paralysis.

Pathophysiology of Hyperkalemia
Potassium is one of the most important electrolytes circulating in the body, having effects on multiple organ systems. Cells within our body create a perfect balance of storing majority of the potassium within the cell and allowing a regulated amount to be circulating plasma volume. While many patients in the hospital tend to need supplemental potassium for low levels (hypokalemia), this post is going to be covering what happens when patients have high levels of potassium (hyperkalemia). Hyperkalemia can be fatal if not recognized and addressed quickly enough. The reason it is so deadly is because of its effect on cardiac cells (cardiomyocytes) and potential for fatal arrhythmias. In fact, a potassium-rich solution (cardioplegia) is used during cardiac surgery to stop the heart from beating during cardiopulmonary bypass.

OSA: Screening and Diagnosis
Obstructive Sleep Apnea (OSA) is a common breathing disorder characterized by partial or complete closure of the upper airway while sleeping. These episodes are usually associated with frequent night time wake ups from hypoxemia and hypercarbia. It is estimated to occur in around 13% of males and 6% of females, however many overweight people go undiagnosed. OSA tends to be higher in the surgical population compared to the general public. It can also be associated with comorbidities such as hypertension, ischemic heart disease, pulmonary hypertension, congestive heart failure, stroke, arrhythmia, and insulin resistance. Upper airway obstruction is likely to happen more frequently and for longer periods of time after receiving anesthesia. Postoperatively, patients with OSA have a higher risk of atelectasis, pneumonia, pulmonary embolism, delirium, atrial fibrillation, and ICU transfers. For these reasons, it is vital to screen for and appropriately manage patients with OSA intra- and postoperatively.

OSA: Perioperative Management
Now that we understand the importance and relevance of OSA in surgical patients, let’s review the perioperative management of these patients. Your approach has three phases: preoperative, intraoperative, and postoperative. Each of these moments is an opportunity to reduce the perioperative complications associated with OSA. This can reduce overall health care cost, reduce prolonged hospital stays, reduce ICU upgrades, and make for a better operative experience for the patient.

Common Pacer Modes
Choosing the right pacemaker mode depends on numerous factors. These include the patient’s intrinsic cardiac rhythm, age, exercise capacity, comorbidities, and chronotropic response. The modes can be divided into three categories:
(1) Asynchronous Modes
(2) Single Chamber Modes
(3) Dual Chamber Modes

Cardiac Pacemakers
Pacemakers are an electronic device that are used to maintain and control the rate and rhythm of a patients heart beat. They are used to treat abnormal rhythms (arrhythmias) that are either too fast, too slow, or irregular. Ultimately, they keep the chambers of the heart beating at the appropriate time to ensure adequate flow through the heart. They can be temporary or permanent, depending on the indication for its use. If permanent, the pacemaker device will be placed in the chest wall. The leads of the pacemaker travel through the subclavian vein and into the superior vena cava. They ultimately attach to the right atrium, right ventricle, and at times the left ventricle.

Tracheoesophageal Fistula
Tracheoesophageal Fistulas can be a serious and life threatening congenital abnormalities in a newborn. It results from the failure of the tracheal bud to develop normally from the primitive foregut during embryogenesis. There are various ways that the esophagus and trachea can be associated in TEFs. There are 5 most common presentations and are named Types A through E.

Labor Analgeisa
When a patient is in labor, the anesthesiologist has the role of pain relief, which can prevent potential negative maternal and fetal consequences of increased sympathetic activation. Neuraxial analgesia has proven to be most effective and is the most common form of pain relief for laboring women. Of neuraxial techniques, generally speaking epidurals are most commonly used for vaginal deliveries and spinals are used for cesarean sections. During labor, pain originates from different spinal levels depending on the stage of labor.

Coronary Disease in Noncardiac Surgery
When taking care of a patient requiring surgery who had a recent heart attack, there are three main things to consider before bringing them into the operating room: When was their heart attack? Was there any intervention? Are they on dual antiplatelets? If the surgery is emergent, that supersedes these questions and you continue to the OR. If the surgery can wait weeks to months, then you need to assess when it would be safest to proceed. Once in the operating room, it is the Anesthesiologist’s job to maintain a balance of myocardial oxygen supply and demand to reduce any further injury or ischemia to the heart.

Cardiac Disease and Anesthetic Risk Assessment
Cardiovascular disease is one of the leading causes of death worldwide and is the #1 cause of death in the US. Cardiac complications in patients undergoing non-cardiac surgery is a major cause of morbidity and mortality in the perioperative timeframe. This risk can be as high as almost 10% in patients with multiple risk factors. As anesthesiologists, it is our role to make sure that we reduce this risk as much as possible. This starts with a preoperative evaluation of each surgical patient and determining if they are safe to proceed for their given operation.

Prematurity and Associated Pathologies
Prematurity is defined as an infant born prior to 37 weeks gestation. Premature infants can be further subdivided by their birth rate: low birth weight (< 2500 g), very low birth weight (< 1500 g), and extremely low birth weight (< 1000 g). The earlier a baby is born and the lower the birth weight, the higher the risk for morbidity and mortality. There are certain risk factors that increase the likelihood of premature birth related to the fetus, placenta, uterus, and mother. Premature infants have a risk for multiorgan dysfunction due to multiple anatomical pathologies.

Neonatal Assessment
How do we know that a baby is healthy right after birth? The pediatrics team performs an assessment called the “APGAR Score” at minutes 1, 5, and 10 after birth. There are major physiologic changes that happen during the transition of being in the uterus to now living in the outside world. This score helps predict the safety and the need for cardiopulmonary assistance after the baby is born. It was put into practice in 1963 and has remained the mainstay of assessment for newborns almost 60 years later.

Fetal Circulation
Fetal circulation varies from neonatal circulation simply because the lungs are not active in a fetus. A fetus relies on the placenta for gas exchange. Since the pulmonary circulation is unable to provide oxygenation, there are three important shunts throughout the fetal circulation. These shunts are the ductus venosus (DV), foremen ovale (FO), and ductus arteriosus (DA).
