Week 1 in Rwanda
Listen along by pressing play above!
Day 1: Sunday March 5, 2023
Our first full day in Kigali was used to set our team up for success. After sleeping in and waking up to the sun peaking in through the bathroom and the birds chirping outside, we managed to do our first group yoga session in the living room. I got everyone to start the Yoga with Adrienne 30-day series, hoping that we will be able to keep up with this on a daily basis throughout the trip. It seemed like everyone was pretty into it from a mental and physical aspect. For me, these yoga series with Adrienne help me accomplish a few things: carving out time to take care of myself, allowing guided meditation to channel positive energy, and becoming silent to hear the sounds around me in a foreign place.
After we got ready for the day, Dr. Asher was very excited to show us one of his favorite coffee shops - Question Coffee. One of the first signs you see when you enter the shop is “Powered by Women”. It is an NGO sponsored coffee company that employs and empowers women in the community. We ordered some coffee and pastries and got to embrace the true Rwandan coffee experience of sitting and enjoying your coffee with company and in the ambiance of the cafe. This is in contrast to our American culture of grabbing our coffee on the go, ready for the next thing on our to-do list. Sitting outside with Shyamal and Sara, we ate, drank, and soaked up the sun and views before continuing on our way.
The big purpose of the day was to get familiar walking around the city and neighborhoods, get SIM cards for our phones, and get a few snacks for the apartment. We started walking up a hill that didn’t seem to end until we got to the center of the city. It was here that we got flagged down by a man in an MTN vest (the local phone company) who walked us over to an area with some more MTN workers that were able to provide us with and activate SIM cards. It still awes me hearing Dr. Asher talk in Swahili and with an African accent as he interacts with the locals. And then is almost immediately able to go back to speaking with an American accent with Sara and me.
After getting our phones situated, we went to the mall to pick up some items for the apartment. Once our tasks were completed, we made the trek bacj home, which was luckily (mostly) downhill.
Once we got home the plan was to fit a run in around the neighborhood. I introduce Sara and Shyamal to the dice-rolling game “Farkle”, which we played for a little while as the sun started to come down and the temperature cooled off. Around 5pm we mustard up the energy to start our run. We initially went down hill and then up a slight incline as a “warm up” to our run. After that, it was game on. We managed to run all the way back to the city center which was about 2.5 miles from our apartment. On our way back, we added an extra loop that got us home right at the 5 mile mark. To be honest, this was about twice as far as I was expecting us to run given the amount of hills, their intense incline, and the heat. But we banded together, persevered, and everyone felt accomplished at the end.
After showering up, we got ready for dinner time. Our first stop was a bar called “Ikigai”. Shyamal wanted to watch the big soccer game - Manchester United vs Liverpool. Unfortunately his team got destroyed by Liverpool, 7-0. But shortly after our arrival, a power outage made the experience much more memorable. I even learned a new trick of dripping some wax from a candle onto a table to create a stand for the candle to attached to and stay upright. After having a drink, we trekked up to Khana Khazanna - an Indian restaurant that Shyamal had been raving about all day. This may have jinxed his experience for the evening. Even though the menu had an overwhelming amount of options (over 200 items to choose from), the food that we ended up ordering was all incredible. Unfortunately, Shyamal caught something of a stomach bug that Sara and I seemed to have evaded. We chalked it up to his fruit juice that he ordered with dinner. We eventually made it home after our late dinner, not really knowing how this was going to affect Dr. Asher going forward. We were all hoping for the best - a quick 24 hour GI bug that would leave as quickly as it came.
Day 2: Monday March 7th, 2023
Today was the start of our work/teaching at CHUK (Teaching Hospital of Kigali). I woke up to a text from Shyamal asking if we could text our taxi driver to drive us to the hospital this morning. The walk to work is about 35 minutes, pretty much all up hill with 3 very steep hills along the way. Our original plan yesterday was to be able to walk to work every morning. But it seemed like the fruit juice that he had with dinner last night wasn’t treating him so well, thus leading us to taxing up to the hospital for our first day.
The difference in the city from Sunday to Monday was like night and day. There was a lot more traffic today (cars, motorcycles, people walking) than there was yesterday. Sundays are pretty much reserved for church and family time, so the streets were pretty empty. But today, we either hit rush hour, or the norm is just to be inches from the vehicles in front of, next to, and behind you while driving. I don’t think I could safely keep my hand or elbow out the window of our taxi without worrying about hitting something next to me.
When we arrived to the hospital, we made our way down to the simulation center for the Anesthesia residency academic day. There were about 10 residents and one attending waiting outside of the building for the doors to be unlocked. Many of them remembered Dr. Asher from last year and were excited to see him again. We made some quick introductions and pleasantries outside as the person in charge of the sim center came to unlock the doors so we could start the academic day.
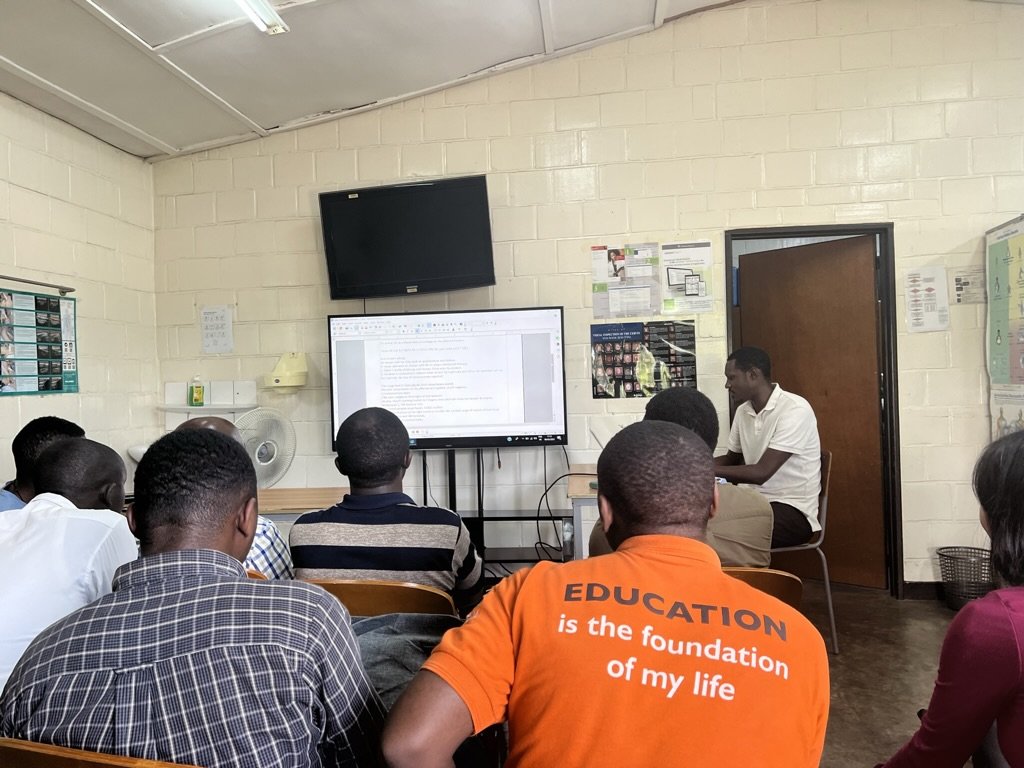
The inside of the simulation center was divided into two room, a lecture room with a TV for projecting slides and a storage room with all the simulation equipment and different types of mannequins. The topics for today’s morning lectures were paraneoplastic syndromes and neuromuscular diseases and their relationship to anesthesia management. The first lecture was given by Theogene. The most memorable part about this lecture was it started with breaking out into two groups and discussing the learning objectives. The point of this was to collect information and then present the information to the rest of the class after about 20 minutes of small group collaboration. This really shifted the ownership of the knowledge base to the majority of the residents, rather than one resident lecturing the class. Theogene’s PowerPoint served as a backup to fill in the gaps that the groups may have missed during their research. Instead of a whiteboard or chalkboard, there was poster paper on an easel. One resident would be the scribe while another resident was presenting the information that was gathered. Everyone was engaged and no one looked like they were upset about what was being asked of them - a notable contrast from what I’ve seen back home.
After this lecture, there was then a case report about a motorbike accident causing an upper extremity injury. The residents went through the preoperative, intraoperative, and postoperative management of the case again using the poster paper to outline what was being discussed. If you looked around, you would also notice residents writing down some of the information in their personal notebook, probably collecting the information to review at a later time. It was so apparent that these residents were incredibly book smart and had the knowledge base for engaging medical conversations. There were times that I was so sure of their confidence based on their previous knowledge that when they would say something wrong I would second guess myself before correcting them.
After our break from lunch, the attending who was there for the day led a Jeopardy session that seemed to be well received by the residents. We broke into two teams and the human nature of competing against each other started to come out. Other than the fact that the team names were Premier League Soccer names, a lot of the mannerisms reminded me of being back home. There was some teasing of the opposing team and trying to steal points at every opportunity. My favorite category was the “Fun Facts” category and the most memorable question from that list was “Which animal has the highest baseline blood pressure?” - It is a giraffe.
After Jeopardy, Sara and I led the residents through a couple of simulation scenarios using the mannequins. The residents were very engaged for this portion. We had one main scenario in mind (esophageal intubation) that ended up flexing into multiple different scenarios for them to work through like main stem intubation, early extubation, larygospasm creating negative pressure pulmonary edema, and having to talk to the family about an unintended anesthesia complication. I think they really enjoyed having to work through the scenarios as a team. One thing that stood out was the observers couldn’t help but creep closer to the scene and start helping their two colleagues who were the ones running through the case. There was a sense of collectivism amongst them, wanting their colleagues to succeed no matter what curveballs or stressors we put on them.
Another particularly memorable portion of the day was Shyamal was still pretty sick all day. He wasn’t really able to keep down any food or liquids in his stomach. Throughout the morning session, he would leave the lecture room to walk around outside. I’m pretty sure there were a few times he was hiding behind trees dry-heaving. At lunch he order some fries and probably ate too many because at the end of our lunch time it sounded like none of the fries ended up remaining in his stomach after his trip to the bathroom. After we were done with our sim and it was time to go home, Sara and I could tell he was in no shape to make the 40 minute walk back home in the heat. So we called our cab driver and had him take Shyamal home. Meanwhile, Sara and I went to the grocery store to try and get some bland food to make for dinner to help him tolerated some sort of food in his stomach. We also exchanged some money and stopped by the bar next to our apartment to have a drink before heading back home for the night. We had some heart to heart conversations on our walk home and at the bar about family life, our relationships, what residency has been like the past 2.5 years, and how we see global health fitting into our future careers.
After getting home, we decided to do some yoga before dinner time. Sara started some rice on the burner and about half way through our yoga session we started to smell something burning. Turns out the rice was cooking faster than expected and started to disperse smoke throughout our apartment. We quickly removed the rice and put the pot outside before finishing the last 10 minutes of yoga in our smoke-filled apartment. Somehow Shyamal slept through all the shenanigans and eventually came out to a slightly less smoke-filled apartment. The only real benefit was it probably smoked out some of the mosquitos that I had accidentally let in the night before after opening up our patio screen door that I didn’t realize was slightly ajar. Since our homemade dinner plans were kind of ruined, we ended up just eating leftovers from dinner the night before and having some snacks that we had around the house. I also taught Shyamal and Sara how to play Monopoly Deal which ended up being a hit once they got the hang of it. We play a bunch of rounds and by the end of the night Shyamal was starting to feel better and gained an appetite for some toast and chips. It was perfect timing to fit the assumed diagnosis of a 24-hour GI bug. Once we eventually got tired, it was time to go to sleep.
Day 3: Tuesday March 7, 2023
Today was our first day in the operating theaters. Luckily Shyamal’s 24-hour stomach bug had subsided and he was feeling well enough this morning to make the 40 minute trek to work. After a light breakfast and coffee at our apartment, we headed up the hills to CHUK. This walk is no joke and inevitably we ended up arriving to the locker rooms sweatier than we started the day. In the locker room, there was a locker specifically assigned for CASIEF volunteers that was stuffed with scrubs, gloves, a couple of white coats, scrub caps, OR shoes, and a bunch of miscellaneous items that I’m sure will become useful when you least expect it. After changing into scrubs, we entered the main operating theater where we met one of the CRNAs, Elie, who showed us around the ORs. He remembered Dr. Asher from last year and of course was excited to see him return.
We walked by the 6 main operating rooms as we made our way to the back of the building where the PACU was located. A couple things stood out during this short walk. Shyamal noted that all of the operating room doors were new and had replaced old, broken doors from last year. The second was many of the surgeries going on were being performed under spinal anesthesia with no sedation. Outside of obstetrics (ie. C-sections), this would be unheard of in the US. But, all of these patients seemed quite relaxed for the situation they were in with low to normal heart rates.. The third thing that was memorable was the anesthesia machine that was in the PACU not only had a halothane canister attached to it, butwhen we turned it on all the words were in Chinese. So without much knowledge of a typical anesthesia machine and where the usual buttons are, you would be completely lost if trying to figure out how this machine works - unless you know Chinese of course.
After our brief tour of the main ORs, Sara and I grabbed some white coats before walking outside to the pediatric operating theater where one of the chief residents was working for the day. We met Guillaume in the operating theater where the staff was turning over the room from the previous case. We stuck around for 2 cases: an EUA (exam under anesthesia) for suspected anorectal prolapse/fistula and a laparoscopic orchidopexy. Both patients were about 4-6 years old. We watched Guillame do the preop evaluation, check the patients labs, induce with a mask induction, and maintain general anesthetic with mask ventilation for the first case and an endotracheal tube for the second case. A big contrast between the adult and the pediatric ORs is the pedi patients were absolutely terrified to be there. They were carried into the operating theater by the nursing staff, kicking and screaming as they were placed on the operating room table. During mask induction, everyone was doing their best to comfort the kids and hold them down until they reached a level of anesthesia that relaxed their muscles and the kicking subsided. The pediatric surgeon had an incredible amount of swagger to him. He was speaking in English to the medical student that was working with him, teaching him how to place IVs after the mask induction. He was also speaking English to his resident and occasionally to the staff in the room. The reason I point this out is because I think he may have trained abroad and came back to Rwanda to practice his skills. He was singing along to his music playing in the operating theater and every move he made seemed to come easy and natural to him.
Around lunch time, Sara and I left the operating theater to get some food with Shyamal. He brought us to the close by neighborhood of Nyamirambo for some shopping and food. This neighborhood was what I imagine most people think Africa looks like. A bit more rural than where the hospital and our apartment were. The houses were more packed and the streets congested with fast moving and erratic traffic. We didn’t see many tourist walking around here. He wanted to swing by the Nyamirambo Women’s Center (NWC) which was a store front that was definitely targeted towards Americans/tourist, considering the prices were in USD. But it was a cool place to see - an all-women run business with the goods being made right next door to the store that you could look into and see the process. We all got some gifts for our loved ones back home and them continued on to seeing more of the town. After walking around some more, we popped into another souvenir shop that was run by a Rastafarian. We got some more gifts for cheap here (not tourists prices). After we concluded our shopping, we sat down at a restaurant for some lunch. I ordered the ugali (which seemed to be a popular staple on the menu) with vegetables, not knowing what to expect. Shyamal and Sara had both had it before from their time in Kenya and described it was a thick, cake-like rice but very dense and was used to pick up whatever side dish came with it. It was so dense that you could basically eat is as your only meal for the day and you would be set for a while. Plus it was only $4 so I had to try it. Once it came out, it was piping hot and Shyamal taught me how to cool it down in my hand and then create a little pocket to scoop food up with. It was basically like creating your own scoops chip.
After lunch, we walked back to the hospital to touch base with Guillaume about tomorrow’s plan. They had just finished a colovesicular fistula case for a 4 month old with severe malnutrition (4kg). When Sara and I walked in, they had just extubated the patient and were waiting on a transfer to the pediatric ward. We clarified the timing of morning report tomorrow and asked if he could send us the operating room assignments for tomorrow. I also asked him if he could show us where the ICU was, but after getting a response that didn’t hide his exhaustion from the day I told him we could figure it out tomorrow. I can appreciate how physically and mentally draining a day in a pediatric OR can be. After exchanging phone numbers, we headed out for the evening.
While we were changing in the locker room, one of the attending anesthesiologist introduced himself to us. Turns out he is a regional trained anesthesia consultant and is one of the faculty staff here at CHUK. It was perfect timing as we were looking for point people to hand off the supplies that we brought with us. Before changing out of our scrubs we ended up back in the main ORs with him. He discussed his fellowship training with us and a WFSA conference he was headed to in the next week or so abroad (in India I believe). We then entered an OR with him for an induction of a patient who was getting a large skin graft to his upper extremity after a severe burn. The patient had an EJ line that was used for induction. We checked out some of the emergency medication vials that were in the anesthesia setup area such as ephedrine, epinephrine, and atropine. We also got to see a patient who was finishing up having wrist surgery under a supraclavicular block (again with no sedation, wide awake).
After leaving the hospital, Shyamal wanted to do a little more shopping for his son on our way home. We ended up stopping at a store that had multiple vendors selling similar souvenirs but we found one vendor that was selling Rwandan soccer jerseys. We ended up all getting a shirt and wearing them out to dinner that night. We went to a restaurant called Heaven, which Shyamal was very vocal about not being excited about. He had gone last year and said it is overpriced for what it was. But it was on our way home and seemed like a reasonable place from the outside to at least try out. But ultimately he was right - we were paying American prices for slightly better than average African-style food. We definitely have had much tastier meals for a fraction of the cost. But this evening wasn’t defined by the food, it was more memorable for the conversations that we had. We all bonded over our upbringing, all having Asian parents, and struggling through the mental weight of appeasing our parents while furthering our careers and adapting to the rapidly-changing world around us. The twist of the conversation was hearing Shyamal’s perspective of becoming a dad and how much thought goes into ever decision you make for your child. We discussed how dinner time is a great time to connect with your family, especially with the unpredictable schedule of working in medicine and having late and overnight calls scattered throughout your weeks. Shyamal mentioned a way to organize your thoughts and get every one talking at the dinner table by discussing a “Rose - Thorn - Bud”: something good that happened, something not so good that happened, and something you are hoping for.
After leaving the restaurant, we were close by our apartment when we passed Ikigai, our neighborhood bar. It sounded like there was live music coming from inside so I convinced everyone to check it out. Once we got inside, we found the singer who was walking around with a microphone, singing songs in multiple different language. We saw lyrics on the TV and anticipated this was karaoke. Shortly after getting our drinks, he started playing “Perfect” by Ed Sheeran, one of my favorite songs. We were all singing along. I started taking a video and one of the bartenders, Eric, who recognized us and knew our names grabbed the phone from my hand and started walking around the restaurant recording the singer and us as we sang along. Not too long after this song, Sara requested the performer to play a Sauti Sol song, one of Shyamal’s favorite bands. He played the song “Isabella”, a beautiful song that Shyamal knew every word to. He grabbed the second microphone and started singing along at our table. This was the perfect way to finish off our long day before walking a short 2 minutes down the hill to our apartment.
Day 4: Wednesday March 8, 2023
This morning we were moving with pace up the hills to the hospital. We were on a mission to make it to morning report with the anesthesia department at the hospital before the surgical cases began for the day. Morning report is when the overnight resident presents an interesting case that came in overnight.
The case that was discussed today was a traumatic brain injury from a motorcycle accident - a very common mechanism of action that lands patients into the operating room. The program director, Dr. Francoise, was leading the discussion after the resident presented the case. She called on various residents and medical students to answer questions related to head injuries, Cushing reflex, and management of increased intracranial pressure. One of the points that Dr. Francoise pointed out and drove home to her residents was that it isn’t enough to just know what happens with the Cushing reflex, but why it happens. This lead to a good discussion of the glossopharyngeal (CN IX) and vagus (CN X) nerves and how they lead to bradycardia from increased blood pressure sensed by the aortic and carotid baroreceptors.
After morning report, we headed to the operating rooms. Sara headed to the pediatric operating theater where a 4 month old was having bladder reconstruction surgery - this was projected to be an all day event. Shyamal and I bounce around the main operating theaters, teaching the residents and medical students who were around. The first case that I was in was a 6 month old getting a VP shunt. One thing that stands out about their pediatric cases is that there are no pediatric fellowship-trained Anesthesiologists in these cases, but the generalists are taking care of sick tiny patients. And they do an amazing job at it. The airway was not straight forward for this case and involved multiple looks with the laryngoscope and eventually downsizing to a 3.5 unruffled tube to fit through the vocal cords. Although the resident seemed a bit nervous (honestly I would be too), the attending and CRNA in the room were relaxed and handled the situation with ease.
As the rest of this case proceeded, we found the UGH medical students to do some teaching with. I was mostly working with a medical student named Fred. He was incredibly book smart. I went over the layers you pass through with a spinal needle, as well as dosing, types, and characteristics of local anesthetics that we use. He pretty much knew all the answers to my questions. When I asked him what he wanted to go into, he told me Internal Medicine because of how much thinking and intelligence it takes to be an IM physician. I encouraged him to consider a future in Anesthesiology and possibly even Critical Care medicine to fulfill the urge of IM. It was just another example of how smart these students in Rwanda truly are.
Before we took a break for lunch, one of the attendings told us about a POCUS workshop that would be taking place on Thursday and Friday and asked if we would be willing to help out. Of course we jumped on the opportunity since this was something that we were already trained in and were extremely passionate about. Another attending had flagged Dr. Asher down to let him know that there was a thoracic case going on today for an empyema washout. Shyamal told him that we actually had brought double lumen tubes with us but that they were back at the apartment. The attending offered Dr. Asher to borrow his car to go pick up the tubes but given how crazy the traffic is in Kigali, it didn’t seem like the best move. He had offered me up to go literally run back and grab the tubes for the case, but the attending ultimately decided that they would do the case on another day.
After some tea time for lunch, we headed to the ICU where we met up with Theogene. He seemed very busy at the time that we found him, finishing up paperwork and signing orders for nurses. So we briefly chatted with him and then started to walk around the ICU on our own checking out vent settings and infusions. As we were walking around, Theogene ended up joining us and discussing a few of the sicker patients in the ward.
One of the conversations we had was about sedation, specifically for a patient who was post-craniotomy. The sedation they use in the ICU is called “KFM” - ketamine/fentanyl/midazolam. The doses are either 100mg/100mcg/10mg per hour or 50/50/5. Although, in this case they left out the ketamine to reduce any harm or excitation to the brain. We discussed the concept of context sensitive half life with fentanyl and the potential accumulation of midazolam with renal failure and how these patients may take 12-24 hours to wake up after you discontinue this infusion. We then started talking about our sedation practices in the US which is usually propofol or dexmedetomidine. We also discussed propofol-related infusion syndrome which can lead to a lactic acidosis, renal failure, and oddly enough green-tinted urine.
Once we were done chatting with Theogene, Asher and I walked home for the day. We were determined to get another run in on this trip and this seemed like a good evening for it. So once we got home, we changed and found a route that was going to be take us to new parts of the city. Once we got running up the first hill, we were dying. The first part of the run that was only steeply uphill turned into a walk-jog-walk some more. Once we hit the flat portion, we picked up some speed and headed to the roads behind the Marriott. Now traveling downhill, we found some new restaurants and cafes, saw the other side of the Presidential Palace, and found the building sites of some new-age condos. Outside the palace stood armed guards and at one point we were running towards their direction. One guard started to remove his hat and I immediately told Asher we should turn around - I didn’t think the optics looked favorable in our position. In another part of town, we passed a Montessori school where Asher stopped to take a picture to send to his wife, Saima, for future reference.
After showering off, we started working on our QI project that was going to be implemented during the 2-day POCUS course coming up. Sara and I made worksheets for the residents to write their answers for the pre- and post-test. Shyamal worked on the presentation portion of the exam that would be displayed in the front of the classroom. It contained 4 images, each with 5 questions including “name this view” and “identify the structures labeled”. Shyamal took over the DJing for the house and was playing Sauti Sol while we finished up our work before heading out for dinner
For dinner, we went to a restaurant called Bistro cafe. It was located on the third floor of a hotel and the views from the windows of the city were incredible. The food was also quite good as well. We learned a lot about Shyamal during dinner like his father’s business, a restaurant that he used to go to as a kid in Kenya that opened up a location in Chicago, and his obsession with fantasy football that has since toned down. When we first got to Bistro, we had talked about going to the roof top bar. But at the end of the night, we all decided that we were too tired and wanted to go home. Asher pulled out another MBA lesson and talked about the Journey to Abilene - a story about a family that ends up going to a place they think they all want to go to but once they arrive they realize everyone is miserable. The lesson is if one person spoke up, they may have all realized they were all thinking the same thing that was different from the original plan. Moral of the story - we headed home after dinner and enjoyed an early bedtime before our busy day tomorrow.
Day 5: Thursday March 9, 2023
Today was another education day with the residents. There were two visiting Anesthesiologists from Poland who were invited to give an ultrasound workshop over the course of two days. This worked out perfectly for us for two reasons - (1) we had Shyamal with us who is a Cardiac Anesthesiologist and co-taught our POCUS curriculum back home and (2) the Rwandan residents were very excited about learning and using ultrasounds. When we first got to the hospital, some of the residents were waiting outside of the simulation center for the doors to be opened. We had brought a few double-lumen endotracheal tubes with us to Rwanda which proved to be useful because they had a patient on the OR schedule who was going to get a thorascopic washout for a lung empyema. When we started showing the residents the DLTs, Dr. Asher immediately went into teaching mode and started going over the basics of single lung ventilation. As residents were arriving, they gathered around as we discussed how the DLTs work to selectively ventilate the left or the right lung.
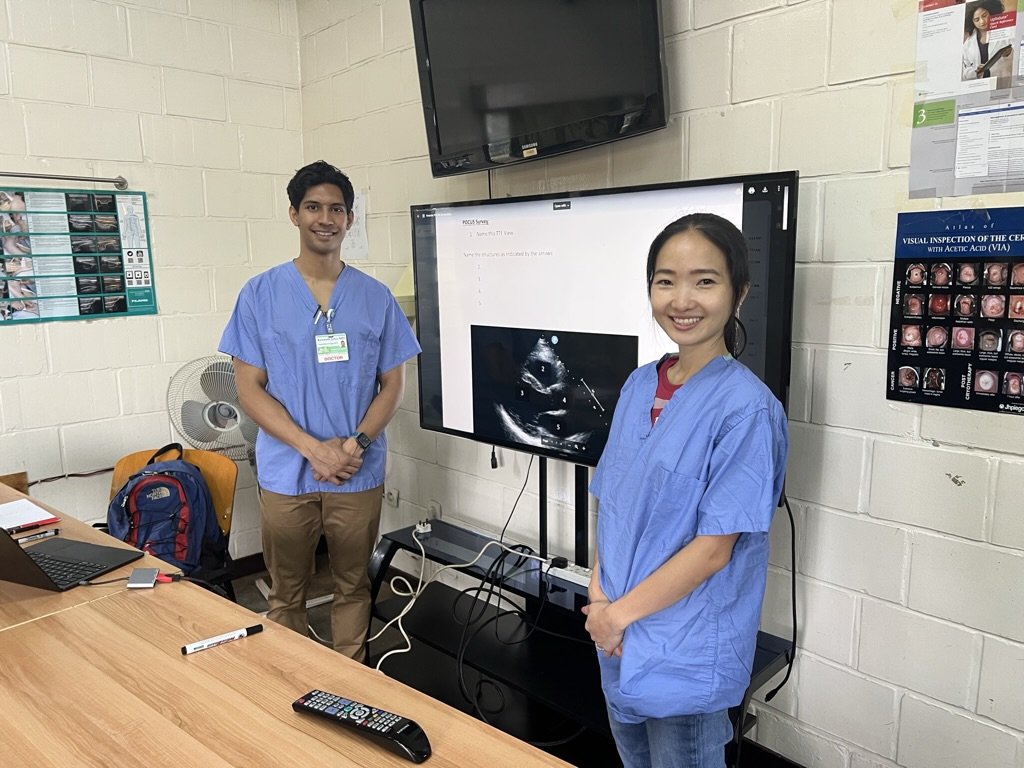
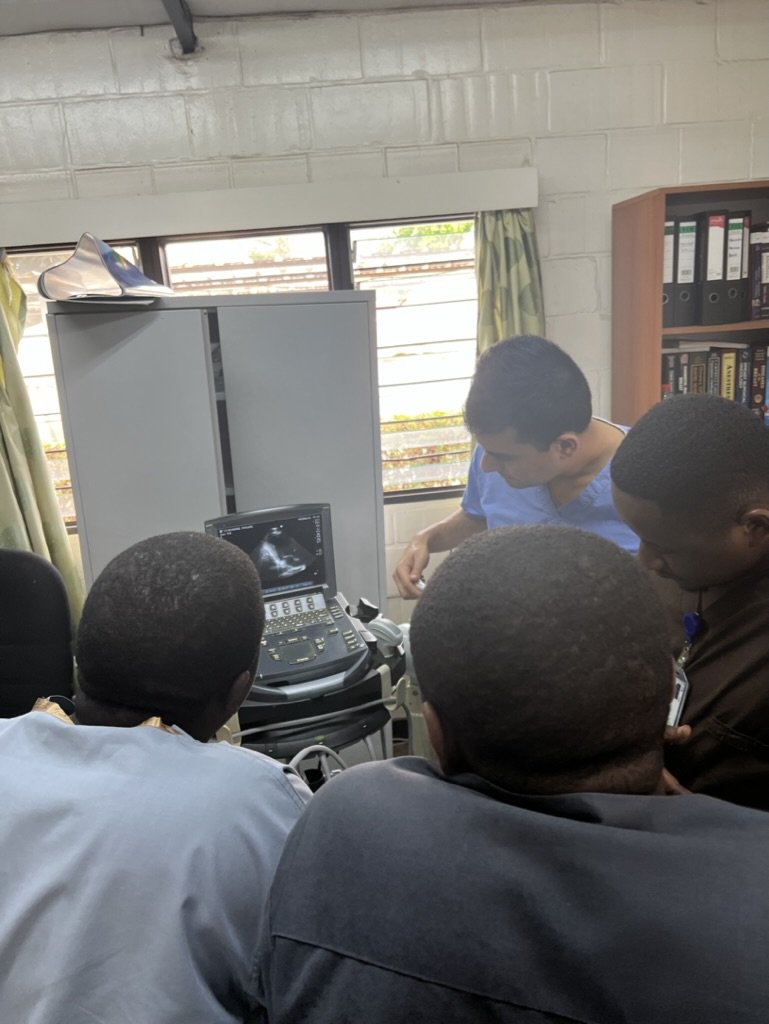
Once the doors were open, Sara and I set up our cardiac POCUS images. Luckily the guest speakers were running late so we were able to administer our pre-test to the 10 residents before the workshop officially started. Once the residents finished the test, the speakers still were not there so Sara and I started doing “chalk talks” on their poster board and easel set-up, discussing why we use cardiac POCUS, the 6 etiologies for hypotension, and the determinants of myocardial oxygen supply and demand. The guest speakers eventually showed up towards the end of our talk and began their own PowerPoint presentations on eFAST and lung ultrasound. After each presentation, the residents would break out into two groups to scan the patient models that were there for the day.
The guests from Poland brought a couple portable ultrasounds that we really good quality. Good enough that you could see the bladder filling from the ureters when scanning the pelvis. There were two patient models and the residents scanned from both sides. The three of us split up between the various groups to walk each resident through scanning the lungs, abdomen, and pelvis. They were all so eager to get their hands on the ultrasound probe. When we were scanning the lungs, Raymond (PGY2) showed me pictures of a case he had where his patient had the absence of lung sliding and ended up having a pneumothorax. He said the reason he knew what he was doing was from Googling it but was never formally trained on lung ultrasound. Didn’t really seem to matter - his intuition and resourcefulness got him to the proper end point.
When it was time for lunch, Shyamal wanted us to come to the OR with him because one of the consulting anesthesiologists was requesting his opinion about a case of a 50ish year old woman coming in for submandibular gland surgery who previously had an event of cardiac arrest when she had the other side operated on. We went to the operating theater where she was already on the OR table and the staff looked ready to proceed. After a quick POCUS assessment, there wasn’t anything overtly wrong with her heart. There were no records from the previous surgery either to help fill in the details of the cardiac arrest. Ultimately the consultant anesthesiologist did not feel comfortable proceeding without a post-operative admission plan and cardiology work up. The patient’s case was canceled and she was admitted to the hospital. As we walked away from the ORs, the three of us discussed how we would’ve handled this case in the US and the negative consequences of canceling a case especially from the patient’s perspective and everything they had to do to get to this point.
We quickly had some lunch in the attending tent as the residents started to head back into the classroom. Eating in the attending tent was a special occasion for the residents and our group. Shyamal was saying they never got to do this last year. And the food was pretty good too! Hot and fresh African dishes like rice, beans, beef stew, and potatoes. Once we returned into the classroom, we finished up some cardiac physiology chalk-talks as we waited for the Poland guests to rejoin the group. Then the rest of the afternoon was spent scanning whatever the residents were interested in. I first led my group through vascular scanning for IV and arterial access, looking first at the internal jugular and then at peripheral sites. Then we moved on to scanning for regional blocks, going through the 4 brachial plexus sites, TAP blocks, and ESP blocks. The models had great anatomy to demonstrate the difference between transverse process and ribs/lungs when scanning for the ESP block, with just a slight change in the angle of the probe.
Once we wrapped up scanning for the afternoon, we invited the residents our for some dinner and drinks. They picked out a place called Germany Butchery that was a 5-10 minute walk from the hospital. They all seemed very excited to be hanging out outside of work. After learning more about their personal stories, it doesn’t sound like this happens often. Mainly because they all have families with kids at home, some of whom live up to 3 hours away from work. So when the opportunity came up, they really jumped on it. And it was a blast hanging out with them and seeing them interact and joke around in a nonclinical and nonacademic setting. This was evidence that you can really connect with people over food and drinks. As residents slowly dispersed to make their buses home for the evening, we wrapped up the bill and headed to our next event for the night.
Jackson was one of the graduates from the CHUK Anesthesia Residency and knew Dr. Asher from the VAST (simulation) courses in Canada. He invited us out for dinner at Great Wall of China. We got in a taxi and made our way to a part of town we hadn’t seen yet. It still amazes me how much Asian influence there is in the Rwandan cuisine. When we arrived, we found Jackson waiting for us. He had finished a busy day of sedation cases at KFH (King Faisal Hospital) before meeting up with us. The food was pretty good but the conversation was the best part of our evening. Jackson is a fun, interesting, and humble guy to talk to. He talked to us about all the places VAST has taken him for simulation courses. His favorite place in the world he has been to was Dubai, where he was visiting one of the global health fellows for under 24 hours. He talked about his time on a boat that traveled around the coast of Europe and Africa that served as mobile hospital stopping at various ports along its path. We also talked a bit about goals for the residency program and how to create a research presence to allow the residents to have publications on their resume once they graduate. After finishing dinner, we said our goodbyes and headed on our way home for the evening.
Once we got home, we played a lot of rounds of Monopoly Deal. Once Sara and Asher tasted victory, they wanted more of it. And since the games only last about 15-20 minutes, it was easy to say “one more game”. Once we finally exhausted ourselves, we headed to bed for the evening to rest up for another full day of POCUS teaching.
Day 6: Friday March 10, 2023
Day two of our POCUS workshop started with morning report with the whole department of anesthesiology. Ironically, Robert was presenting on aortic stenosis this morning. Prior to that, Guillaume presented the overnight cases. It sounded like a very busy night. One of the cases he discussed was a pediatric patient with a bowel obstruction from ascariasis (parasite/round worm invasion of the intestines). He said the patient ended up having an 8cm bowel resection with “milking” of the rest of the bowel to remove any residual infection. Without getting into too much detail, he said there were thousands of parasites that were ultimately removed. Unfortunately when patients present with peritonitis from this infection, the mortality is quite high.
Once Guillaume was done, Robert presented his PowerPoint on aortic stenosis. This was a nice set up for the rest of our academic day which was going to be focused on cardiac ultrasound. After his presentation, Dr. Francois had residents consider what type of anesthesia would be safest for a pregnant patient with aortic stenosis who needed an urgent c-section. It was good reminder for everyone in the room that although aortic stenosis can be a scary underlying diagnosis, it is not a complete contraindication for neuraxial anesthesia. Because they do not use arterial lines frequently here, the biggest difficulty would be close hemodynamically monitoring after the sympathectomy from an epidural or spinal.
Today’s ultrasound focus was on the cardiac exam. This was our favorite topic to teach probably because of Asher’s cardiac background and my interest in ICU. The residents were also very excited about incorporating the exam into their rounds in the ICU. We had the same models from yesterday and the younger of the two patients had almost textbook anatomy for the residents to practice on. While we were scanning with the residents, the Poland guests brought small groups of residents to the ICU to scan real patients for potential pathology. For the residents who stayed in the sim center, once they got the hang of the 4 views of the heart, we started getting into more advanced topics like assess for valve regurgitation and identifying the specific cusps of the mitral and aortic valve. Their favorite part of the exam was the subcostal window and assessing the IVC size - a previous group had taught them to use this as a way to assess volume status. The biggest learning pearl I could teach them here was to first obtain the subcostal 4-chamber view then rotating the probe 90 degrees will allow you to see the IVC emptying into the RA. This would help differentiate the IVC from the aorta, which are close in proximity and can be easily confused.
We were scanning right up to lunch. In fact, the last thing I looked at with a few residents was getting a view of the IVC and doing a passive leg raise to see how the preload bolus would affect its size and collapsibility. Since our model was already dehydrated and had a collapsing IVC, the passive leg bolus showed a signifiant difference in the IVC, and the quality of the ultrasound was so good that you could see the flow of volume with the vessel itself. Dr. Francois just happened to be walking by while we were doing this and she was amazed, calling it “magic”. Today I sat with the residents during lunch time and chatted more about our personal lives. They couldn’t believe that I had been married for almost 4 years and had no children. They said that if a couple was married and didn’t have a child within 2 years, people would start to assume that their wife was infertile. It made me appreciate the lack of pressure in my life to have a kid in my current career phase. I also heard about the pay discrepancy for Anesthesiologists in Rwanda compared to neighboring countries where they can make 10x the salary. This usually causes a few Anesthesiologists each year to move out of Rwanda to practice medicine - adding to the disparity of total anesthesiologists available in the country of Rwanda.
After lunch, we distributed our post-workshop quiz to the residents, going over the 4 echo images from the pre-test. After everyone completed the test, we went over the answers as a group. It was clear based on their speed of responses that they picked up some knowledge of the past day and a half and felt comfortable names structures on different echo views. I am hopeful that the hands-on practice will help them incorporate these skills into their patient assessments. Once we wrapped up the echo discussion, I filled in the rest of the afternoon lecture time by going over a case of an elderly woman who fell and fractured her hip requiring who also happened to have aortic stenosis. I wanted to bring back the conversation that started this morning about AS and how we can manage these patients under spinal for an orthopedic case like a femur fixation. We started with the pre-op evaluation which led into intraoperative management of this patient using a spinal technique. I then incorporated some other resuscitation topics like transfusion complications such as TRALI and hyperkalemia. This took us to about the 3pm hour and I could tell the residents were ready to get an early start to their weekend.
Dr. Asher was headed home this evening and I’ll never forget this goodbye speech to the residents. They were all sad to seem him go but appreciative of the time and effort he put into their education this week. “Why do we all love mangos? Would we love them as much if they were available, sweet, and ripe all year long? Probably not. We appreciate the ripe and sweet mangos because you can only get them during certain times of the year. Think of me like that mango. It’s easy to appreciate moments like this when they happen seasonally.” The residents had a riot with this speech.
As we walked outside, he whispered in my ear “that mango thing just came to me, but I think my African connection really came through there.” He was 100% correct.
As Shyamal and I walked back to the apartment for the last time together, we decide to stop at Hotel des Mille Colline to have one last debrief together. This was the hotel that the movie “Hotel Rwanda” was based on. After seeing the movie, the location holds a lot of emotional weight in my eyes. As we walked to the entrance of the hotel, I had goosebumps on my arms thinking about the scenes in the movie of the buses of volunteers leaving the local Rwandans to hide out in the hotel. As we sat by the pool and had some juice together, I asked him to recap how global health has become integrated into his anesthesia career. Being born and raised in Kenya is ultimately the root of his passion for giving back to Africa. But his first experience with global health is ironically being not selected to travel to Kenya with the ASA global health initiative when he was a Brown Medical student. The irony came to life when he was selected to be the at large representative for the ASA global health committee a couple years ago. Then there was an opening to become the US chair for the CASIEF foundation, who is responsible for this project in Rwanda. The theme I was picking up on was things fell into place when the timing was right and he was able to ultimately able to position himself in a position to feel proud of his work without forcing anything. This was also the theme for this past week - without forcing anything and allowing flexibility, we found ourselves in very rewarding positions where our knowledge and skills were valued.
Day 7: Saturday March 11, 2023
Finally the weekend had arrived. I was getting quite exhausted towards the end of the week. It felt like I had been on-call all week, only getting around 3-4 hours of sleep per night between the jet lag and wanting to keep up with journaling/posting updates at night time once everyone went to bed. Sleeping in this morning was really nice and the rest of the day was going to be focused on moving at a relaxed pace.
After getting ready for the day, I headed to Question Coffee to grab some breakfast and take advantage of a beautiful place to do some journaling. There were significantly more people there than we had seen a week ago when we first arrived. Specifically, there were a few kids who seemed to be European or American based on their accent. Their parents were also around but the kids seemed pretty independent in terms of entertaining themselves. I overheard two kids talking about a friend of theirs who was also coming to Rwanda. One of the girls said, “You know how we can make someone feel special? We can make a sign for them at the airport that say ‘WELCOME TO RWANDA!!’”. The selflessness and incite in these kids was unparalleled.
Once finishing up breakfast, I got a day-pass at one of the hotels in the city center to get some exercise in. Included in the day-pass was access to the locker rooms with a sauna, hot tub, and shower to rinse off in. After showering off, I spent the rest of my time at Kigali Serena journaling more (I had some incomplete memories from the weekdays that I wanted to go back and complete). I also was able to compile some pictures/thoughts for Twitter and videos to make short reel about the POCUS workshop we helped with. Twitter apparently became a great resource to not only connect with the residents of CHUK but also with physicians associated with Stanford Anesthesia who had visited Rwanda as well.
When I left to Serena, I walked to another part of town to have a quick bite to eat before picking up Danny from the airport. On my walk, a man came up to me and started having small talk with me. Once he realized I was from the US, we started talking about basketball. He talked to me about his love for the Chicago Bulls and the Michael Jordan teams. We then started talking about Steph Curry and the Warriors being the more famous team in the present day. Once I got close to my location, I slowed down and stopped in front of the shopping mall. That’s when he started to tell me that he was picking up him HIV medicine from CHUK and was on his way home but was hoping that I could buy him a juice concentrate for his family that they could use for the next few weeks. His story and our interaction was different than the typical begging you encounter walking around, so I felt inclined to help him. After buying him a couple bottles of the juice, we went our separate ways but not before he graciously thanked me for my small act of kindness. The thing that stuck with me the most was he expected people from my country to be shutoff to people like him and not give him the time of day. This left me somewhere between sad and proud of the interaction we had. Even if you want to see this story as someone targeting me and using me for my money, this simple act of kindness was worth more than the $15 that I spent on juice for his family. In my view, providing food and drinks to someone is a good compromise for helping random people who are asking for money.
I eventually reached a location that I thought would be “The best Nigerian Food in Rwanda” based on my google maps. However, this location turned out to be a soccer bar where people were piled in watching the Leicheister vs. Chelsea game. After looking at the menu, I order a beer and some fries while I watched the game. Unfortunately, the fries were taking a considerable amount of time to come out and at a certain point I had to leave in order to make it to the airport on time. But the views of the city from this top floor bar and watching Rwandans enjoy soccer and play pool was a priceless scene.
Once I got back to the apartment, Cyrill picked me up to head to the airport to pick up Danny. I brought my safari hat and a sign that said “WELCOME DR. DANNY BUI” on it as a welcome inspired by the two girls at Question Coffee this morning. Right outside of the airport, Cyrill and I both had to get out of the car and walk through a security booth with a metal detector while the vehicle went through a security checkpoint that resembled something similar to a carwash. This was my first time going to the airport so I had no idea what was going on or that we were close to the airport. After getting back into the car and driving 30 second into the airport parking lot, I realized that this was an airport security check point. Unfortunately Danny did not see me holding my sign amongst all the people awaiting FIFA conference attendees. He took an early turn and didn’t walk past where I was standing. But after he called my phone we quickly found each other and headed back to our neighborhood to meet up with Sara.
We went to Bistro for dinner, our second time at this restaurant. One funny realization was that with Danny we could order meat dishes and have family style dinners where we can pass around and share each entree without any dietary restriction. After a yummy dinner at Bistro, we headed towards our favorite neighborhood bar, Ikigai for karaoke night.
We knew based on our last time there for karaoke that Saturday evening was another night that it would be happening. When we got there, it started pouring hard, so we ended up staying longer than we initially intended. But the best part was the later we stayed, the more we head local Rwandans sing karaoke and it seemed like everyone that sang was a professional singer. One girl sang Alicia Keys “Everything’s Going to Be Alright” and I swear it was better than the original. Not too long after she sang, Sara went up to her and they quickly became friends. Eventually after realizing that the rain was not slowing up anytime soon, we decide to scurry our way home and get drenched in about 5 minutes of rain until we were in the comfort of our apartment.