Physiological Changes During Pregnancy
This will be a review of majority of the physiologic changes that occur during pregnancy involving the neurologic, cardiovascular, respiratory, gastrointestinal, renal, endocrinology, and hematology systems. It will also review anesthetic changes/considerations to have when taking care of a pregnant patient.
Starting with the central nervous system, there are three key points to hit here: sleep, cerebral blow flow, and sympathetic nervous system. Pregnant patients have increased insomnia and day-time drowsiness. Cerebral blood flow is increased steadily throughout pregnancy. And patient’s have an increased reliance on their sympathetic nervous system for hemodynamic stability.
With the cardiovascular system, the biggest change is an increase in cardiac output. This is the result of increased contractility and increased heart rate. Other cardiac changes can be seen on echo or EKG.
The respiratory system sees an anatomical change, creating a restrictive lung pattern. However, pregnant patients have a higher minute ventilation. This causes a slight respiratory alkalosis throughout the pregnancy.
The gastrointestinal system is first affected by the positional change of the stomach. This change in position leads to the high rates of GERD. Hormonal changes lead to a decrease in gastric motility and nausea. If symptoms of nausea and vomiting persist, this is known as hyperemesis gravidarum.
The kidneys experience changes during pregnancy due to increase circulating plasma volume. The GFR will be increased leading to decreased serum creatinine and BUN. It is normal to see increase protein and glucose urinary excretion.
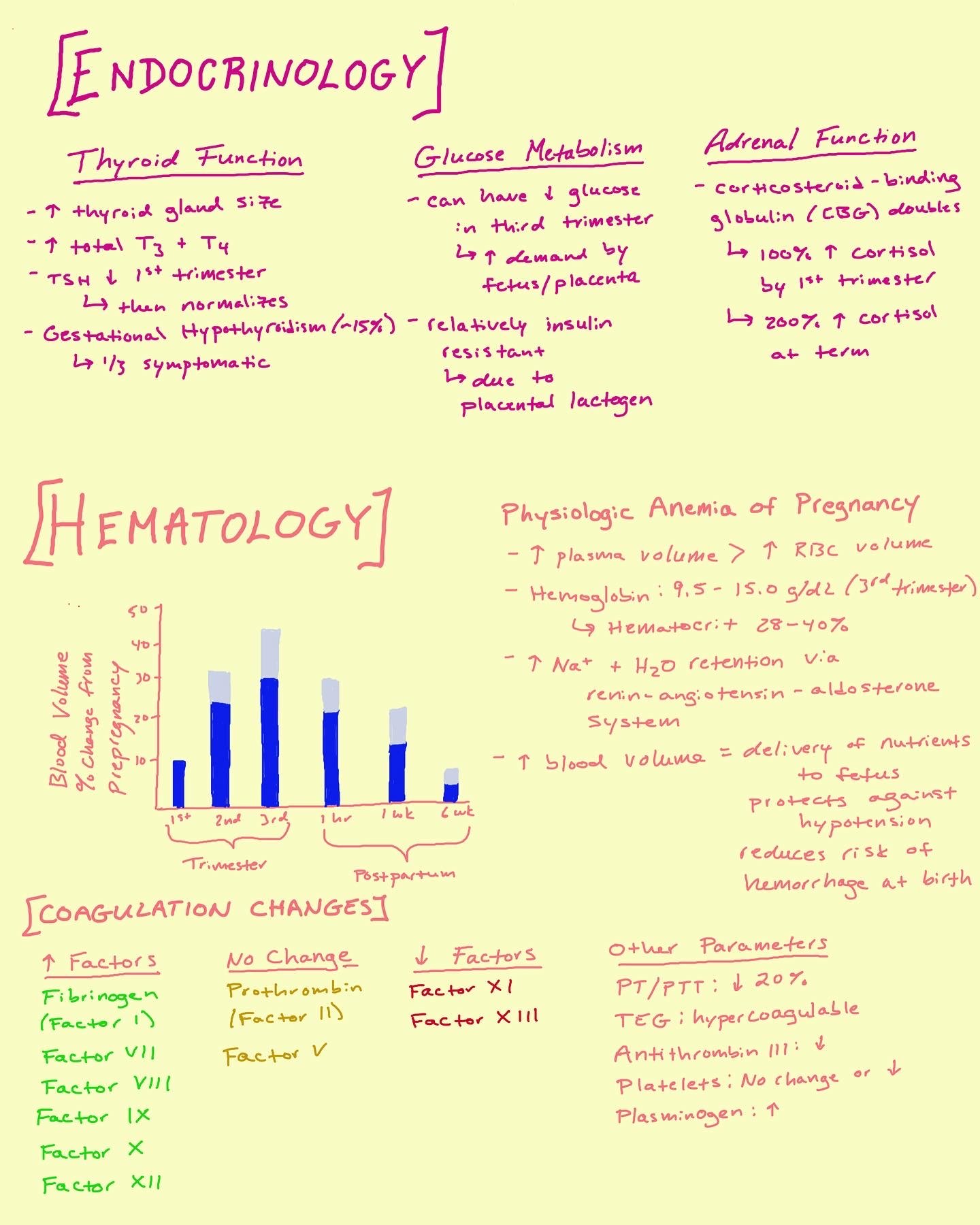
For endocrinology, we can break down the changes during pregnancy into 3 categories: thyroid function, glucose metabolism, and adrenal function.
Lastly, we’ll cover hematology. These changes can be divided into two sections: blood volume and coagulation. Ultimately, both create protective mechanisms against hemorrhage at birth.
Whether you are doing general anesthesia or neuraxial anesthesia, there are adjustments that can be made to your anesthetic plan.
Treatment of hypotension after a spinal or epidural involves 3 main actions: IV fluids, increased doses of phenylephrine or ephedrine, and left uterine displacement to relieve any aortocaval compression.